Transforming Cancer Detection: The Role of Advanced Blood Tests and Key Innovations
The landscape of cancer detection is experiencing a profound evolution, significantly driven by the advancement of blood tests for cancer risk. These pioneering tests represent a revolutionary step forward in identifying potential cancer markers within the human body, thereby facilitating earlier interventions and drastically improving patient outcomes. To effectively navigate the complex and often challenging realm of cancer diagnostics, it is crucial to gain a thorough understanding of both the fundamental principles underlying these tests and the latest innovations emerging in this vital field.
Diving Deep into the Science Behind Blood Tests for Cancer Risk: Comprehensive Overview
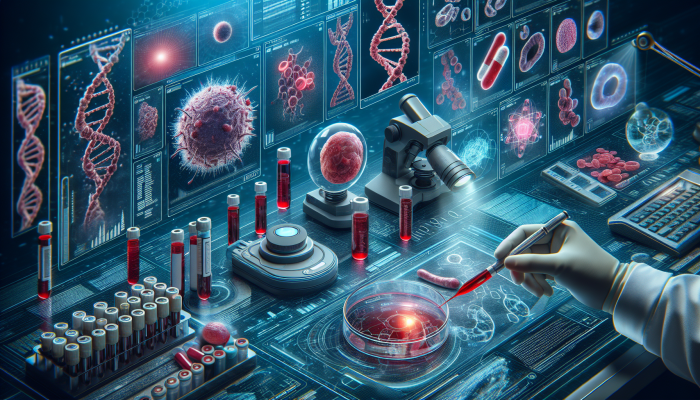
At the core of blood tests for cancer risk lies the critical detection of specific biological indicators known as biomarkers. These biomarkers serve as essential signals indicating the presence of potential cancer or an elevated risk for developing it in the future. They encompass a wide range of substances, including proteins, genes, and various other materials produced either by cancerous cells or by the body as a response to the presence of cancer. The scientific basis for these innovative tests relies on advanced methodologies that accurately identify these markers, employing a diverse array of cutting-edge technologies.
One of the key methodologies utilized in these assessments is the liquid biopsy. This technique involves the analysis of a blood sample to detect components such as circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs). The non-invasive nature of this approach enables a comprehensive evaluation of a patient’s cancer risk without the need for more invasive procedures like traditional biopsies. Furthermore, technological advancements, particularly in next-generation sequencing (NGS), have greatly enhanced the sensitivity and specificity of these tests, making it possible to identify even the smallest traces of ctDNA.
The accuracy of blood tests for cancer risk is intricately linked to our understanding of cancer biology. Different types of cancer release distinct biomarkers into the bloodstream, which fuels ongoing research aimed at discovering new markers that could serve as early warning signals. For example, prostate-specific antigen (PSA) levels are frequently monitored to assess prostate cancer risk, while the CA-125 marker is commonly associated with the detection of ovarian cancer.
Additionally, the integration of artificial intelligence (AI) into the analysis of test results is significantly transforming this field. AI algorithms possess the ability to process vast datasets, revealing patterns that may remain undetected through human analysis, thus greatly enhancing the predictive capabilities of these tests.
Unveiling the Latest Breakthroughs in Blood Tests for Cancer Risk: Essential Insights
The field of blood tests for cancer risk is currently witnessing extraordinary innovations that have the potential to redefine cancer screening and prevention strategies. A particularly noteworthy advancement is the introduction of multi-cancer early detection (MCED) tests. These revolutionary tests are designed to identify multiple types of cancer from a single blood sample, thereby significantly minimizing the need for invasive procedures and enhancing overall patient comfort.
Recent studies have demonstrated that MCED tests can successfully detect cancers in their earliest stages, often before any clinical symptoms become apparent. This early detection is vital, as it correlates directly with improved treatment outcomes and higher survival rates. For instance, a study published in a leading oncology journal highlighted the remarkable ability of an MCED test to identify malignancies that are typically difficult to diagnose early, including pancreatic cancer and ovarian cancer.
Another significant development in this realm involves the exploration of methylation patterns present in circulating DNA as a diagnostic tool. Alterations in methylation are frequently indicative of cancerous processes, leading researchers to investigate how these patterns can be utilized for more precise cancer risk assessment. This innovative technique could provide a highly sensitive means of detecting malignancies for which effective screening protocols are currently lacking.
Furthermore, collaborations between technology firms and healthcare providers are driving the creation of novel diagnostic tools. These partnerships focus on leveraging big data and machine learning to enhance blood sample analysis, resulting in more accurate risk assessments and personalized management strategies for patients.
Understanding the Revolutionary Impact of Liquid Biopsies on Cancer Detection and Treatment Strategies
Liquid biopsies represent a groundbreaking advancement in the domain of blood tests for cancer risk. Unlike traditional biopsies that require invasive tissue samples, liquid biopsies offer a minimally invasive alternative that can be performed repeatedly, allowing for continuous monitoring of cancer progression or treatment responses. This capability is particularly advantageous for patients who may not be suitable candidates for surgical biopsies.
Liquid biopsies function by isolating and analyzing ctDNA or CTCs obtained from a blood sample. The ability to track these cellular components provides valuable insights into tumor dynamics and potential genetic mutations that may occur throughout the disease process. For example, identifying specific mutations can guide oncologists in selecting targeted therapies, thereby personalizing treatment plans for enhanced therapeutic effectiveness.
The incorporation of liquid biopsies into clinical practice is already demonstrating significant promise. Recent clinical trials have shown that these tests can detect recurrences in patients who have previously undergone cancer treatments, often several months prior to traditional imaging methods. This timely detection can lead to prompt interventions, ultimately improving survival outcomes.
In addition, liquid biopsies enable real-time monitoring of treatment responses. By assessing ctDNA levels during therapy, healthcare professionals can evaluate the effectiveness of the treatment regimen and make necessary adjustments. This proactive approach to monitoring signifies a substantial shift towards more dynamic management of cancer care.
In summary, blood tests for cancer risk, especially through the application of liquid biopsies, are revolutionizing the field of oncology. Their potential for early detection, ongoing disease monitoring, and personalized treatment strategies positions them as invaluable tools in the enduring fight against cancer. As research and technological advancements continue, the prospects for these tests to improve patient outcomes and reshape cancer care remain exceptionally promising.
Stay Connected: Join Us on Facebook for the Latest Updates!




Your exploration of advanced blood tests for cancer detection highlights a crucial shift in how we approach diagnostics, but I wonder about the ethical implications of such innovations. While earlier detection can lead to better outcomes, these tests might also create anxiety or uncertainty for patients, especially if the implications of biomarkers are not fully understood or contextualized.